4 Musculoskeletal Anatomy
4.1 Body level concepts
4.1.1 Gross and Microscopic Anatomy
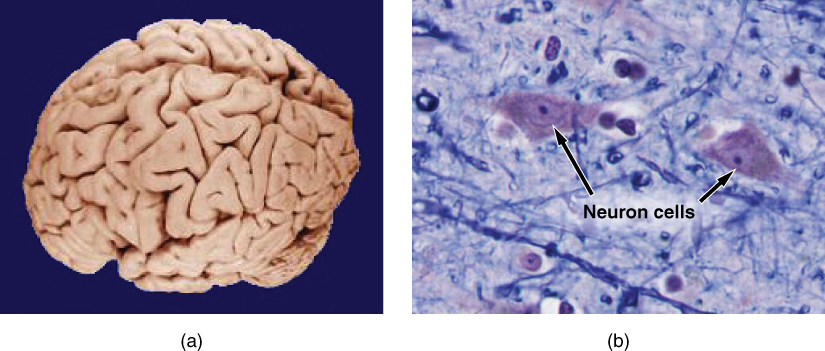
Gross anatomy considers large structures such as the brain.
Microscopic anatomy can deal with the same structures, though at a different scale. This is a micrograph of nerve cells from the brain. LM × 1600.
(slide credit: @OpenStaxAnatomy2020)
4.2 Levels of Structural Organization of the Human Body
The organization of the body often is discussed in terms of six distinct levels of increasing complexity, from the smallest chemical building blocks to a unique human organism.
In engineering terms, it is a multi-scale system
(Modified from: @OpenStaxAnatomy2020)
4.2.1 Organ Systems of the Human Body

Organs that work together are grouped into organ systems.
(Modified from: @OpenStaxAnatomy2020)
4.3 Anatomical Terms
4.3.1 Directional Terms Applied to the Human Body
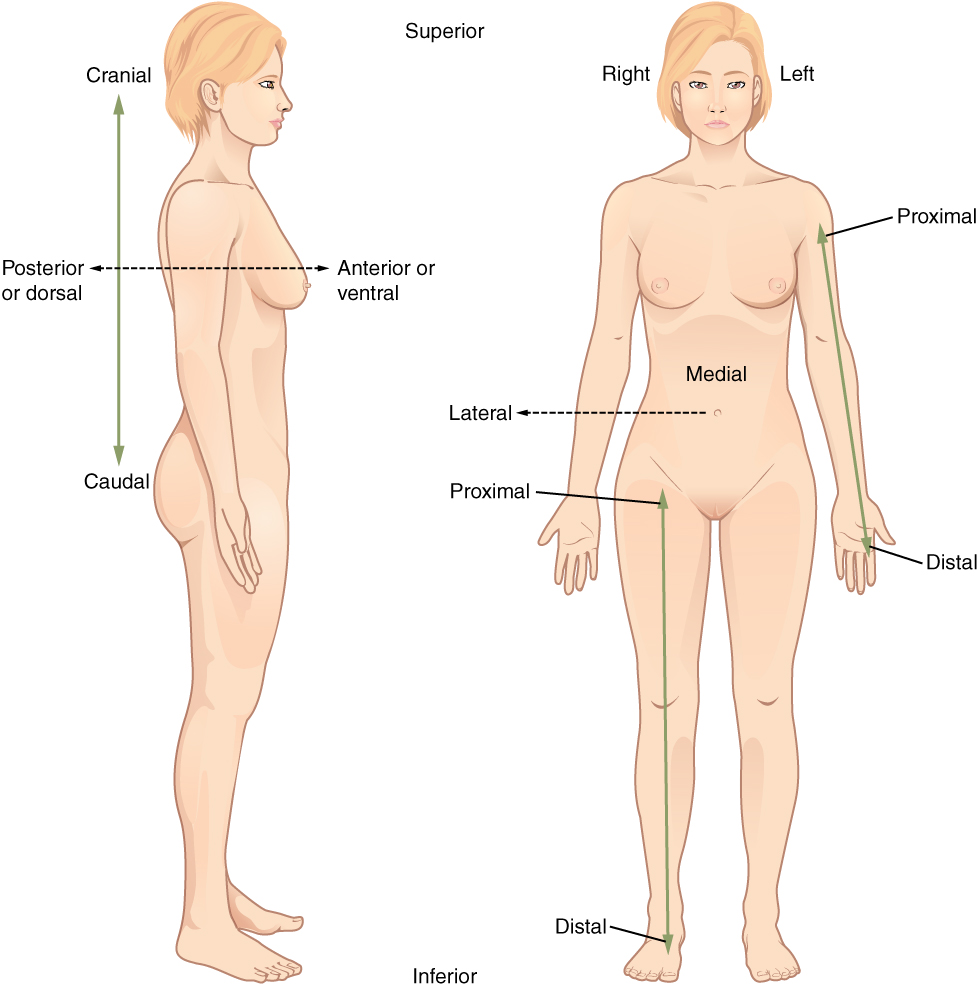
Paired directional terms are shown as applied to the human body.
(slide credit: @OpenStaxAnatomy2020)
4.3.2 Planes of the Body
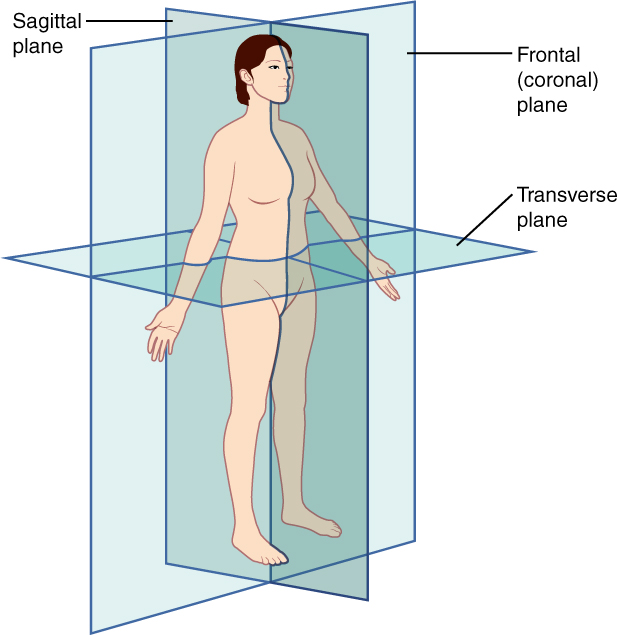
The three planes most commonly used in anatomical and medical imaging are the sagittal, frontal (or coronal), and transverse plane.
(slide credit: @OpenStaxAnatomy2020)
4.3.3 Relative reference terms
- Proximal/Distal aspect
- Nearer to/Further from the origin or attachment point
- Inferior/Superior
- Beneath/Above: Often used in the axial skeleton
- Cranial/Caudal
- Towards/Away from the head
- Lateral/Medial
- Closest to the outside/inside relative to the mid-line in the coronal plane
- Anterior/Posterior
- In front/back (relative position)
- Dorsal/Ventral
- On the back/front
4.3.4 Terms of action
- Flexion/Extension
- The anterior angle between two bones is decreased/increased (except for knees/toes, then posterior angle)
- Abduction/Adduction
- Movement away from/towards the body mid-line in the frontal plane
- Lateral flexion
- Left/right movement of the spine in the frontal plane
- Supination/Pronation
- Rotate the forearm palm forward/backward in the anatomical position
- Dorsiflexion/Plantar flexion
- Rotation of the ankle toes up/down in the sagittal plane
- Inversion/Eversion
- Rotation of the foot up and in/up and out in the frontal plane
- Hyperextension
- Movement beyond anatomical norms
4.4 Principal functions of the musculoskeletal system
Critical functions of the bones
- Hematopoiesis (formation of red blood cells)
- Mineral storage (99% of body’s calcium)
- Insufficient calcium intake thus leads to:
- a reduction of calcium storage in the bones and a corresponding reduction the bones’ “mechanical properties”
- an increased fracture risk
- Insufficient calcium intake thus leads to:
- Protection of the vital organs
- Support and motion
4.4.1 Hematopoiesis
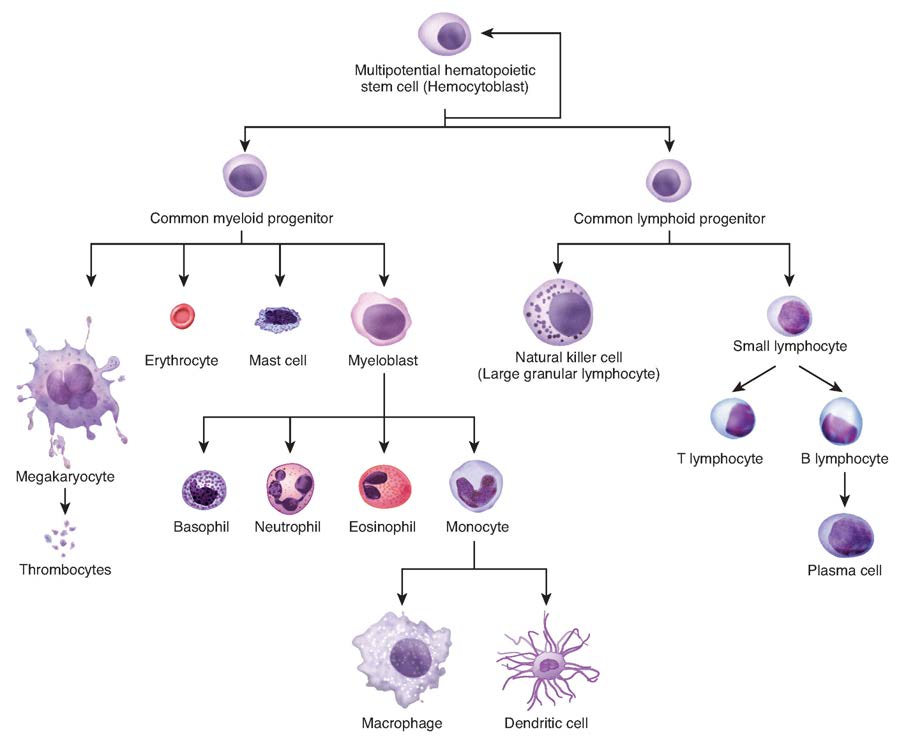
@OpenStaxAnatomy2020 Ch. 3
The process of hematopoiesis involves the differentiation of multipotent cells into blood and immune cells. The multipotent hematopoietic stem cells give rise to many different cell types, including the cells of the immune system and red blood cells.
(slide credit: @OpenStaxAnatomy2020 Ch. 3)
4.4.2 Elements of the Human Body
The main elements that compose the human body are shown from most abundant to least abundant.
(slide credit: @OpenStaxAnatomy2020)
4.4.3 Protection of the vital organs
- Distribute loads (stiff cortical bone)
- Absorb energy (softer cancellous bone)
Examples follow:
4.4.3.1 Bones protect the brain
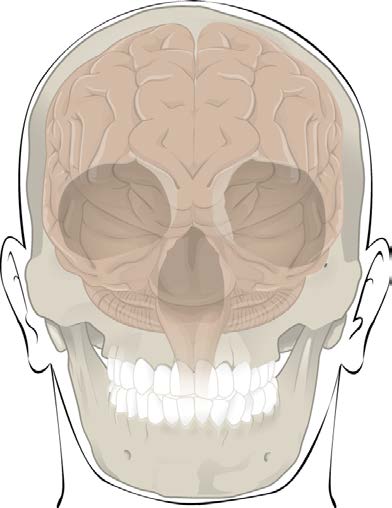
- The cranium completely surrounds and protects the brain from
traumatic injury
- Distributes load and absorbs energy
- Others protective bones
- Ribs, spinal cord, etc
4.4.4 Support and motion
@Bartel2006
- Provide a framework for force and motion necessary for living
- Bone and joints act as levers, muscles act as actuators
- Muscles apply forces at some moment arm, creating torques to rotate a joint
- Consequences of muscle attachment points (relative to joint position)?
- Disadvantage – loads on joints and muscles are larger than the functional loads applied to the body
- Advantage – small muscle displacements cause large rotations and fast motion
4.5 Principal anatomical structures examined to this course
- Bones of the skeleton
- Joints
- Soft tissue
4.6 Bones
4.6.1 Major boney structures examined in this course
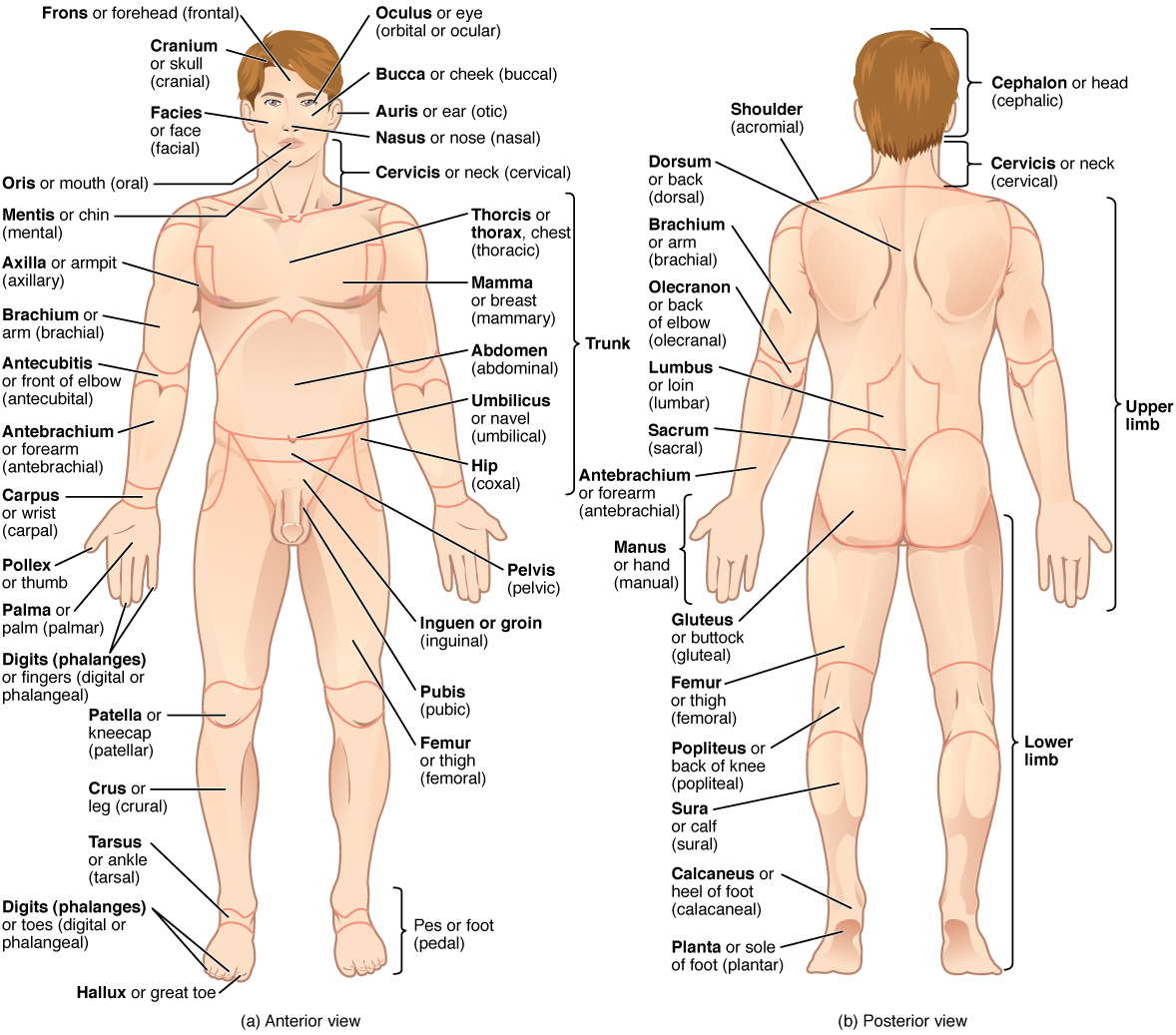
The human body is shown in anatomical position in an (a) anterior view and a (b) posterior view. The regions of the body are labeled in boldface.
- There are typically 206 bones in the human body (+4 sesamoid bones in the foot)
- Can be categorized into roughly 4 groups
- Long bones (femur, tibia, humerus, etc)
- Long in one direction, tubular cross sections
- Short bones (wrist, ankle, hand, foot, etc)
- Have similar dimensions in all directions
- Flat bones (scapula, skull, pelvis, etc)
- Are short in one dimension relative to the others
- Irregular
- Those that don’t easily fit into the other categories
- Long bones (femur, tibia, humerus, etc)
4.6.2 Bone tissue types
Femoral head with metastasis

Femoral_head_with_bone_metastasis
- There are two types of bone tissue
- Cortical (compact) bone
- Dense, stiff, strong
- Load carrying bone
- Cancellous (trabecular) bone
- Less dense, less stiff
- What functions does it serve?
- Cortical (compact) bone
4.6.3 Long bone
@Bartel2006
The shaft (diaphysis) grows from its ends at growth plates (physis)
- The shaft has a medullary cavity filled with yellow marrow (fat and primitive blood cells)
- The proximal humerus and femur have red marrow within their cancellous bone tissue. (Red blood cells are made here)
- The medullary cavity serves no structural purpose in normal bone
- Implants often interface with the medullary cavity as a means of attachment (ie intramedullary nail)
- The epiphysis (bone end) grows from separate ossification centers at the end of the bone
- Metaphysis is the region between the diaphysis and the epiphysis
4.7 Joints
4.7.0.1 Joints can be classified functionally or structurally
- Functional classification depends on the amount of
relative motion… less convenient
- Large motions – diarthrodial joint
- Structural classification depends on joint mechanism
4.7.1 Structural classification of joints
- Fibrous (or Immovable) joints
- Held together by a thin layer of strong connective tissue
- No movement between the bones such
- Sutures of the skull
- Teeth in their sockets
- Cartilaginous joints
- Bones attached by white fibrocartilaginous discs and ligaments
- Limited degree of movement
- Intervertebral discs
- The cartilage in the symphysis (binds the pubic bones together at the front of the pelvic girdle)
- The cartilage between the sacrum and the hip bone
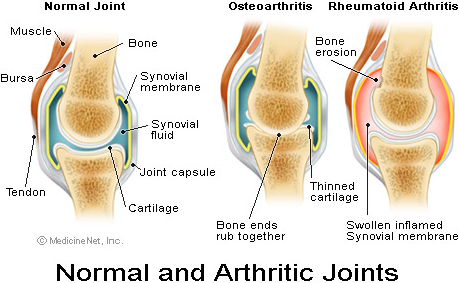
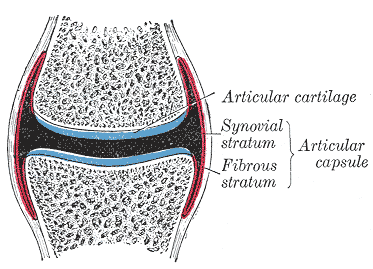
- Synovial joints (subset of diarthrodial joints)
- Covered with a layer of smooth articular (hyaline) cartilage
- Enclosed by a bag-like capsular ligament which constrains the joint and helps contain the synovial fluid
- The capsular ligament is lined with a synovial membrane. This membrane secretes synovial fluid into the cavity as a lubricant
- In addition to the capsule, the bones are constrained by other strong ligaments
- Very low friction coefficient
- human knee – \(\mu=0.005-0.02\)
- human hip – \(\mu=0.01-0.04\)
- Lower than most engineered structures
4.7.2 Synovial joints
@Bartel2006
- Ball and socket
- Condylar joints
- Multiple bone joints (Compound Joints)
4.7.3 Ball and socket
- The rounded head interfaces the cup-shaped socket of another
- Hip
- Femoral head (ball) and acetabulum (socket)
- Shoulder
- Humeral head (ball) and glenoid (socket)
- The glenoid is nearly flat… thus the shoulder requires significant soft tissue for stabilization
- Hip
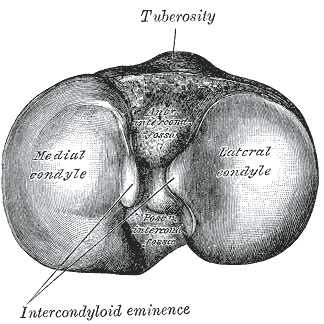
4.7.4 Bi-condylar joints
- The condyles are the enlarged regions at knuckles of any
joint.
- They are enlarged, in part, to minimize the stresses of load transfer.
- Examples: medial and lateral condyles of the femur and tibia
4.7.5 Bi-condylar joints
- “Bi” - Pairs of articulating surfaces
- Two curved condyles articulate against relatively flat surfaces of the mating bone
- There is little kinematic constraint, thus, extensive soft tissue is required for stability.

- Having two condyles allows for resistance to moments in planes
perpendicular to the plane of motion.
- The two condyles and their supporting soft tissues only allow
small angular rotations in planes perpendicular to the intended
plane
- Less muscular restraint required about these planes
- The two condyles and their supporting soft tissues only allow
small angular rotations in planes perpendicular to the intended
plane
- These joints have extensive range of motion in one plane
- ie the knee has extensive flexion/extension in the sagittal plane
4.7.7 Multiple bone joints
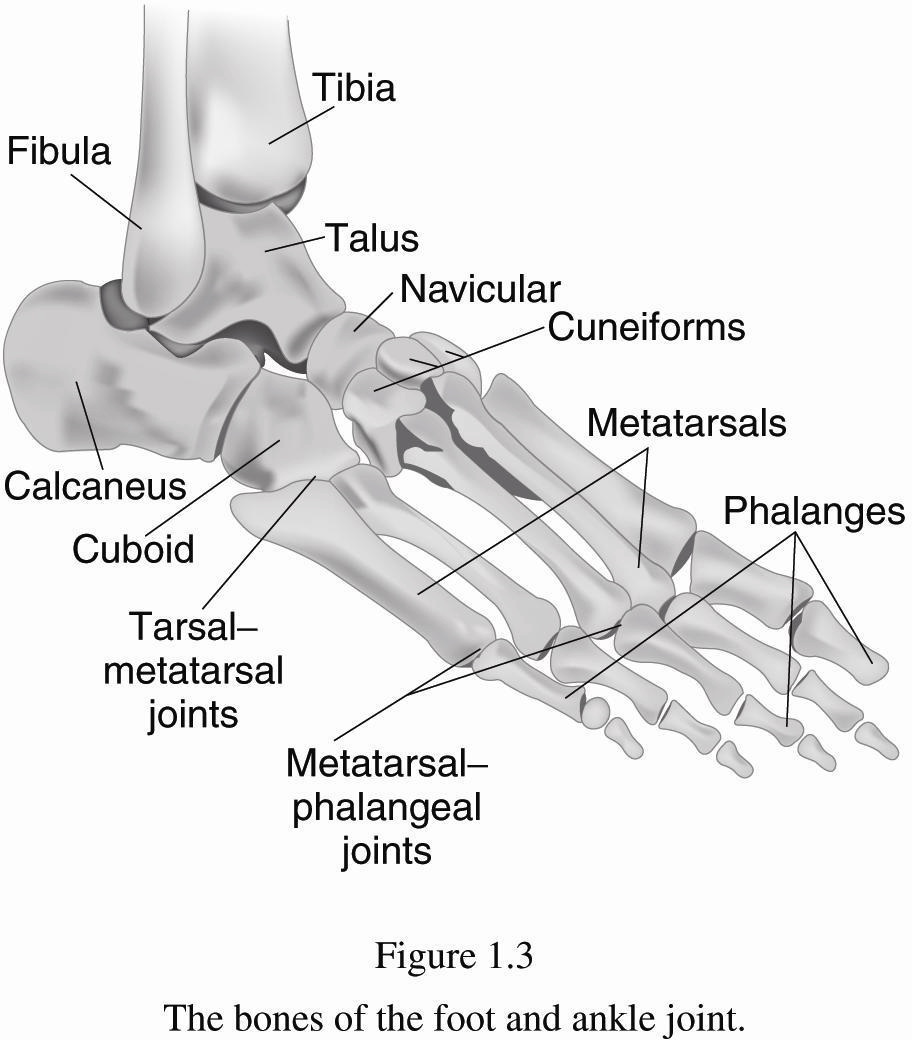
- More difficult to describe than ball-and-socket or bi-condylar joints
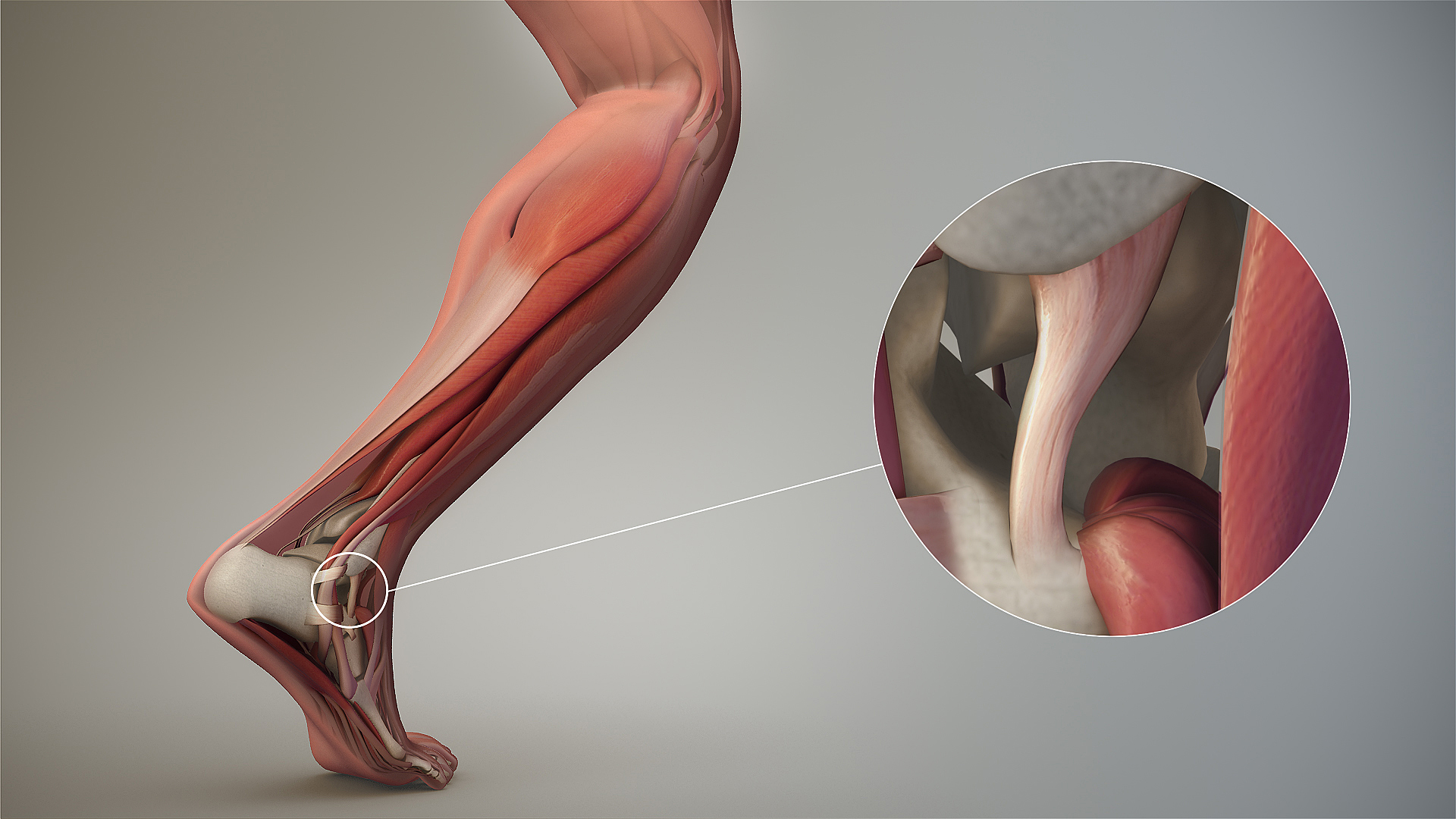
- Examples: wrist (8 carpal bones), ankle (7 tarsal bones)
- Bound by lots of ligaments and have synovial fluid
- Small motions between individual joints add up to larger motions
4.8 Soft Tissue
4.8.1 Soft Tissue
- There are 4 types of soft tissue of interest to this course:
- Muscle
- Tendon
- Ligament
- Cartilage
- We will introduce each of these in this lecture, and each will get substantial treatment (lecture+)
4.8.2 Muscle

- Approximately 700 muscles in the human body
- Three broad classifications
- Skeletal
- Cardiac
- Smooth and visceral (internal to the body cavity)
- Also can be classified as
- Voluntary Striated (skeletal)
- Involuntary Striated (cardiac)
- Involuntary (smooth)
4.8.3 Muscle groups
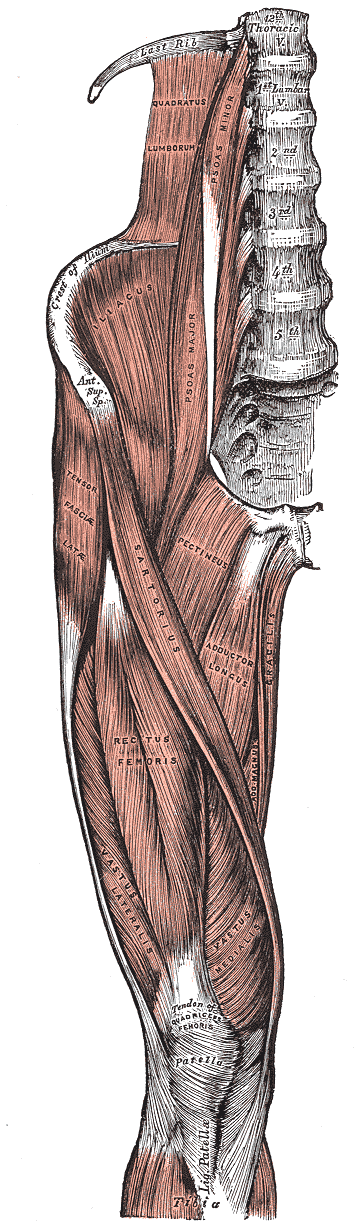
@Gray1918
- In this course, we are principally concerned with skeletal muscles
- These muscles predominately act in groups that have a common insertion point on a bone
- The groups act in concert to provide motion and stability… we
will most often consider the group as a whole
- ie the quadriceps is made up of four muscles
- Muscles groups contract to activate, position, and stabilize the body
- They work in concert with each other, co-contraction of
agonist and antagonist muscles produces joint
control and stability
- Example, the hamstring and quadriceps simultaneously contract by variable amounts to stability the knee joint in flexion/extension

- Muscle contraction leads to forces, forces leads to strains in the
muscle
- Thus, the muscle is also a spring which stores energy
- This is important for energy management within the body
- Note the distinction between strain (injury) and strain (elasticity)
4.8.4 Tendons and ligaments
- Tendons connect muscle to bone
- Ligaments connect bone to bone
- Both can be modeled as simple cables, however, each has tissue bundles at multiple length scales (ie like fibers that join to form a strand, strands join to form a rope)
- When stretched, they deform and have spring like qualities as well
4.8.5 Articular cartilage
- Complex set of tissues consisting of fibrous matrix, water, large molecules, and other elements
- 2-4 mm thick… thickness changes with age
- Note: bursae - Tiny, slippery sacs of fluid which facilitate this gliding motion by providing a thin cushion and reducing friction between surfaces.10
4.8.6

Elbow joint - deep dissection (anterior view, human cadaver) Anatomist90 CCSA3.0
- No nerves or blood supply in cartilage
- Difficult to detect damage
- Does not heal
- Level of detail in the engineering model depends on the desired outcome
4.9 Critical joints discussed in this course
4.9.1 The hip
@Bartel2006
- The hip is a synovial ball and socket joint.
- The head of the femur rotates relative to the acetabulum of the pelvis
- Contact can (sometimes) be modeled as a single force acting
through the center of the joint
- This approximation isn’t perfect
@Bartel2006
- Modeling the hip
- We might model the femoral diaphysis as a hollow circular beam
- The metaphysis can be modeled as an elastic or rigid link, or modeled using FEA if detailed outcome is desired
- Contact in the ball and socket leads to complex load distributions
@Bartel2006
- Muscle attachments to the greater and lesser trochanters
and bony ridges such as the linea aspera
- These allow for a greater moment arm for the muscles
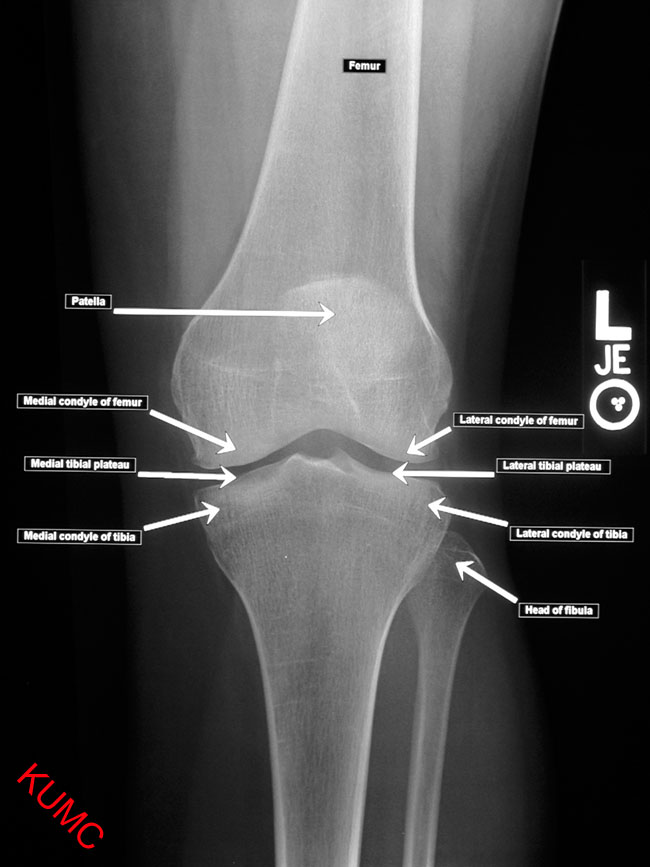
4.9.2 The knee

@Blausen2014
- A bicondylar synovial joint which allows the femur and tibia to rotate, twist, and slide relative to each other
- Each motion is necessary… otherwise abnormal forces develop and cause rapid deterioration of the joint
@Bartel2006
- Important structures include:
- Medial collateral ligament (MCL)
- Lateral collateral ligament (LCL)
- Quadriceps tendon
- Patellar ligament
- Anterior Cruciate ligament (ACL)
- Posterior Cruciate Ligament (PCL)
- Menisci (two crescent-shaped pads that help distribute the loads from the femoral condyles to the tibial plateaus)
- ACL and PCL are within the knee joint capsule and pass through the notch between the condyles, the others are outside the capsule
4.9.3 Spine
@Bartel2006

OpenStax College CCSA3.0
“Cartilaginous” type joint
Connective tissue is a fibrocartilage structure called the Intervertebral disc
Healthy disk acts like a tire… needs to have sufficient fluid inside.
- Aging causes the gel-like fluid to solidify with negative consequences
- Largest avascular tissue in the body
4.9.4 Anterior portion of the intervertebral joint
- Pedicles and laminae form an arch – the vertebral foramen (hole) for the spinal cord


Dr.foksha CCSA4.0
- Adjacent vertebrae are connected through articulating joints (called facets) that constrain the motion between the vertebrae and limit twisting and extension of the spinal column
- The structure supports the upper body and protects the spinal cord.
4.9.5 Vertebral attachments
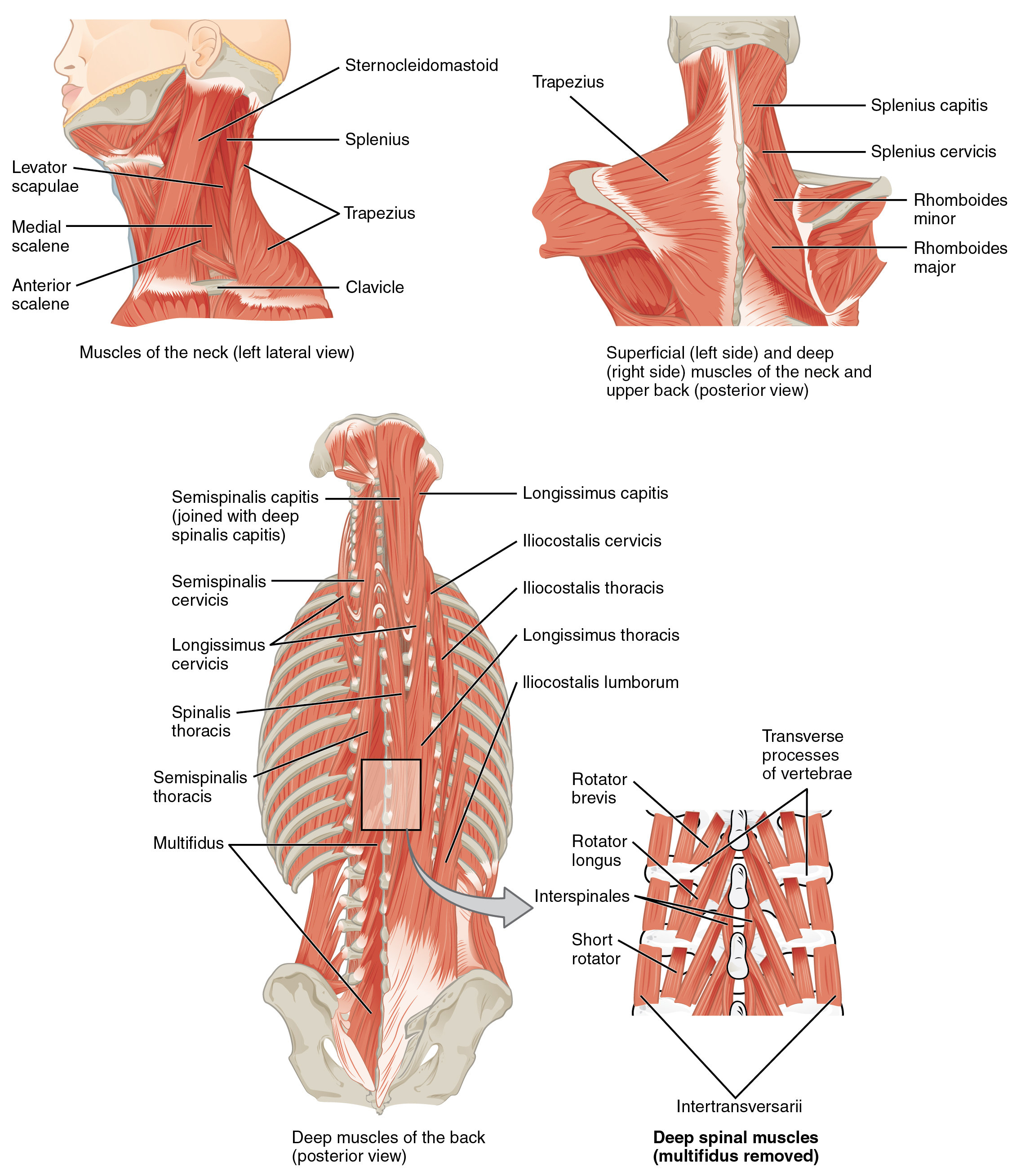
OpenStax College CCSA3.0
- Back muscles attach \(\approx 5\)cm posterior to the center of the vertebral body
- Center of sagittal bending is approximately within the disk
Latissimus dorsi

Anatomography CCSA2.1 Japan
@Bartel2006
4.10 Fracture
4.10.1 WARNING: Traumatic video coming
4.10.2 Fracture
Fractures may occur due to:
- Abnormal loading
- Single traumatic overload
- Cyclic loading which does not overload but prevents healing
- ie stress fracture
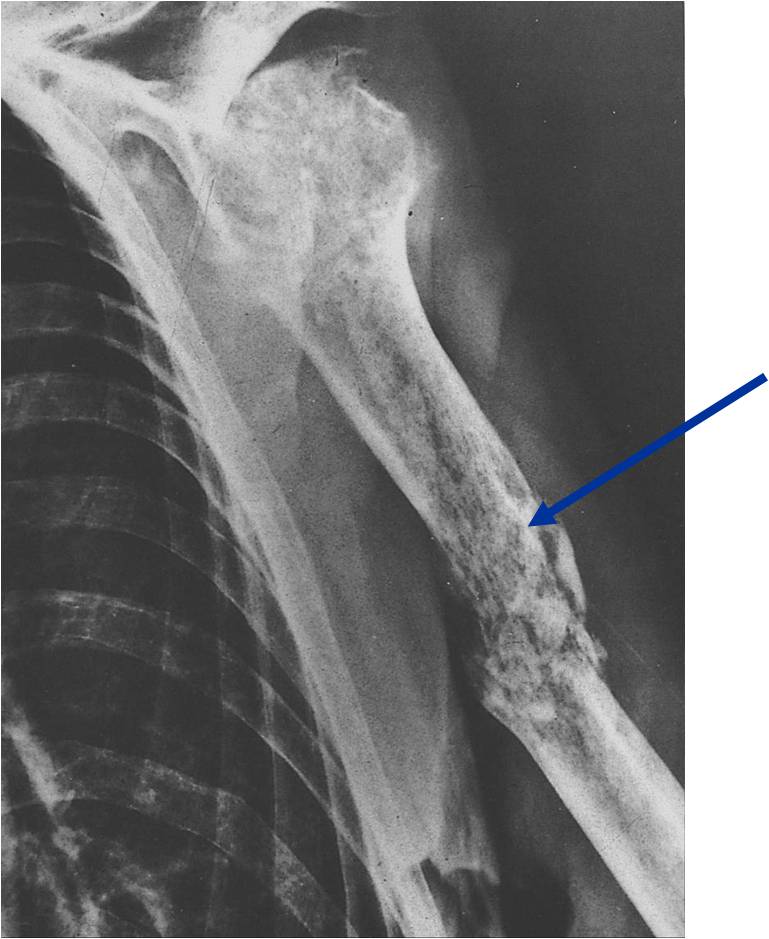
Lymphoma with Pathologic Fracture - http://www.tumorsurgery.org/tumor-education/bone-tumors/types-of-bone-tumors/lymphoma-of-bone.aspx
- Decreased strength due to underlying pathology
- Tumors
- Disease (osteoporosis)
- Lack of use
- Adaption to load demand – prolonged bed red, paralysis, reduced gravity environment, stress shielding by an implant
- Possible project… investigate mathematical models of bone adaptation
4.11 Arthritis
4.11.1 Arthritis
- Deterioration of the joints over time
- Osteoarthritis occurs when some combination of mechanical wear and biochemical degradation erodes the articular cartilage
- It is a localized effect most common in knees and hips
- Damage to articular cartilage may be caused by normal wear, disease, or trauma
- Damage may be direct or due to changes in the subchondral bone
- May also be caused by altered joint mechanics
- ie change in gait due to ankle fusion leads to arthritis in the knee
- Damage may be caused by systemic disease
- Rheumatoid arthritis
4.11.2 Soft tissue damage
- Traumatic loads may cause ruptures of ligaments, tendons, and the menisci
- Damage may occur in the ligament/tendon itself or in the attachment
point to the bone or muscle
- May be entirely within the bone
- The nature of the injury can depend on the rate of loading
- Tendons/ligaments exhibit viscoelastic behavior
4.11.3 Repair
- Musculoskeletal system has an extraordinary ability to repair itself (if the damage is not too severe)
- Bone is continually “damaged” and continually repairs itself
- Damage may be related to the adaption process and necessary to maintain bone density
- Self repair varies with site, tissue, and extent of the injury
- Bone is good at self repair
- Muscle, tendon, and ligament are not as good at self repair
- Severe damage may necessitate medical or surgical intervention
4.12 Visualizing orthopaedic structures
4.12.1 X-Ray of a Hand

@OpenStaxAnatomy2020 Ch. 1
High energy electromagnetic radiation allows the internal structures of the body, such as bones, to be seen in X-rays like these. (credit: Trace Meek/flickr)
(slide credit: @OpenStaxAnatomy2020 Ch. 1)
4.12.2 Computed Tomography Scan

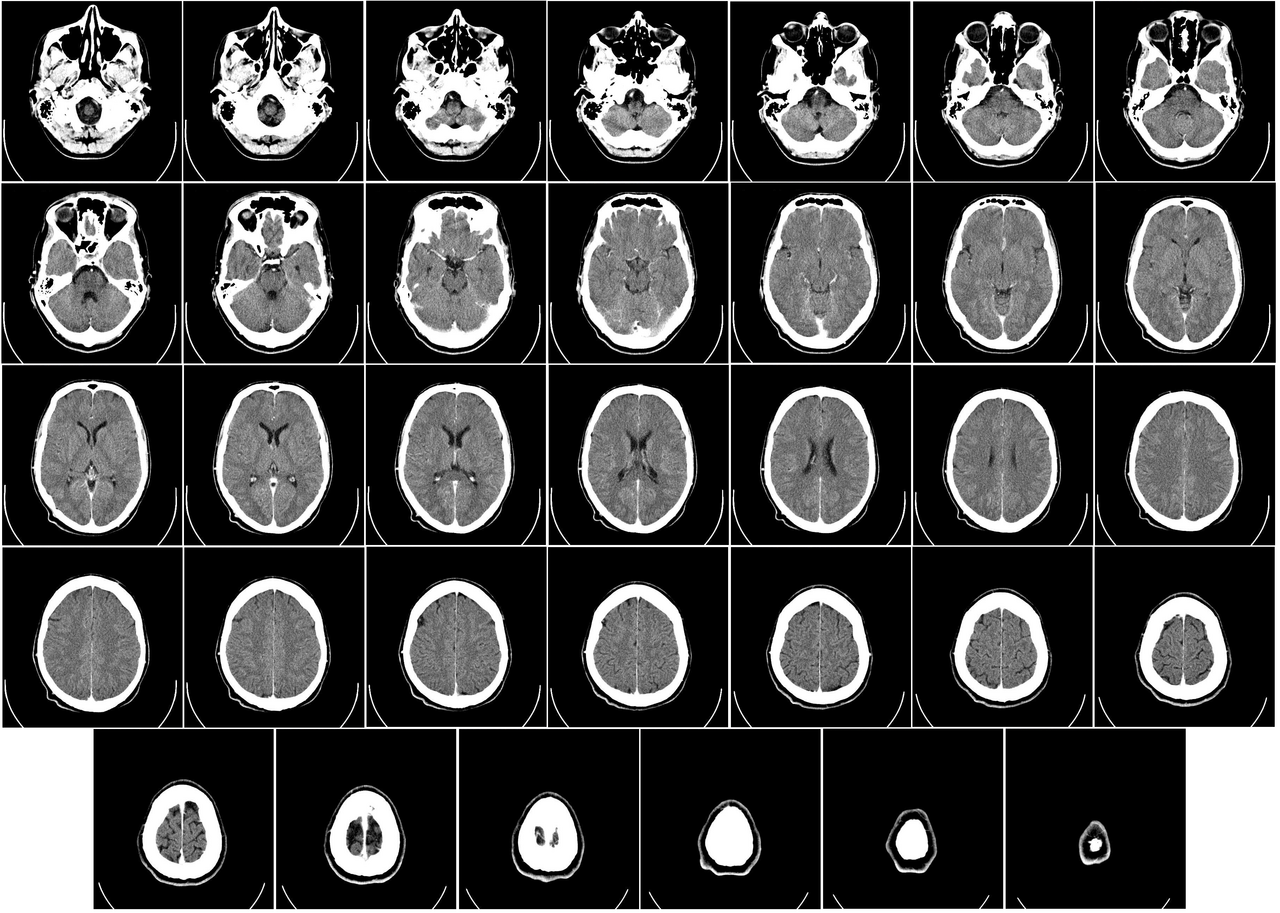
- The results of a CT scan of the head are shown as successive transverse sections.
- Uses ionizing radiation (x-ray radiation)
- Higher contrast visualization of bony structures
4.12.3 Magnetic Resonance Imaging


- An MRI machine generates a magnetic field around a patient.
- Higher contrast visualization of soft tissues
4.12.4 Ultrasound

Ultrasonography is a totally safe noninvasive imaging technique. In contrast to computed tomography (CT) and X-rays, it does not emit ionizing radiation. Unlike magnetic resonance imaging (MRI), it is safe for all patients, including those with cardiac pacemakers and metal implants, without any contraindications.
@Blankstein2011
4.12.5 Ultrasound in orthpaedics
- Can be high resolution
- Can offer real time assessment (i.e., patient can move, image is dynamic)
- Sometimes referred to as the “orthopedic surgeon’s stethoscope”
- Detection of tendon tears, tiny calcifications, and foreign bodies
4.12.6 Positron emission tomography
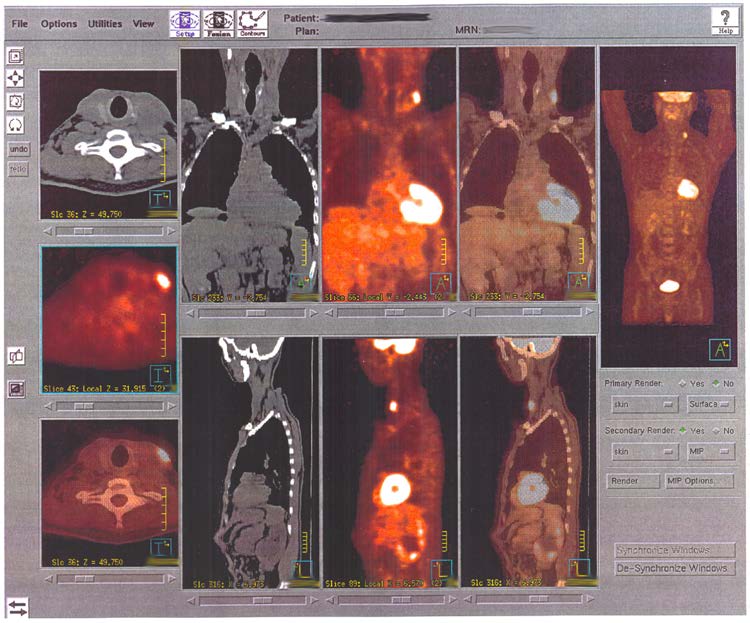
@OpenStaxAnatomy2020 Ch. 2
PET highlights areas in the body where there is relatively high glucose use, which is characteristic of cancerous tissue. This PET scan shows sites of the spread of a large primary tumor to other sites.
(slide credit: @OpenStaxAnatomy2020 Ch. 2)
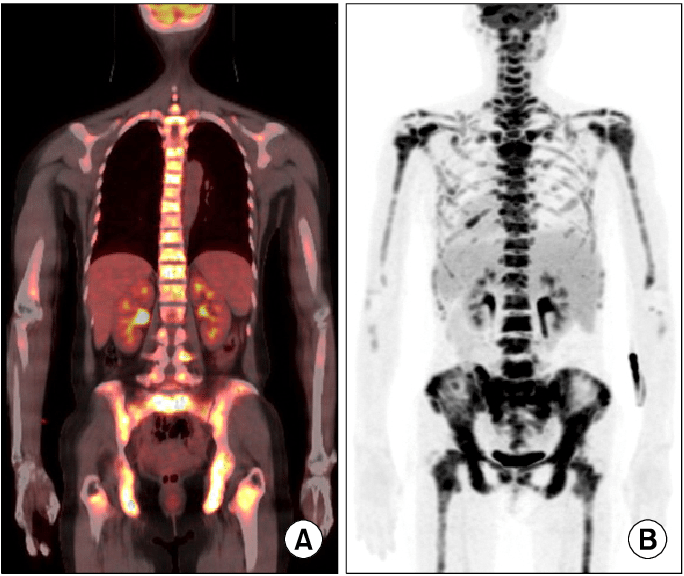
- Can be used to track bone forming activity
4.13 Summary
4.13.1 Objective
To understand the musculoskeletal system well enough to provide engineering support for the treatment of musculoskeletal disorders and for the enhancement of individual and societal quality of life
- Thus, we must:
- understand the basic mechanics or normal, damaged, and repaired tissue and the body structures composed of them
- utilize modern design and analysis tools to improve treatment of disorders
credit a: “WriterHound”/Wikimedia Commons; credit b: Micrograph provided by the Regents of University of Michigan Medical School © 2012↩︎
http://medical-imaging2012.blogspot.com/2012/02/how-to-take-x-rays.html↩︎
https://classes.kumc.edu/som/radanatomy/image.asp?Image=7105-001.jpg&Film=7105&Features=1↩︎
Public domain https://www.needpix.com/photo/929804/muscles-skeleton-half-body↩︎
https://www.arthritis-health.com/types/bursitis/what-bursa↩︎
http://jointhealthworld.com/osteoarthritis/what-is-osteoarthritis-i've-never-heard-of-it/↩︎
http://www.drnickcampos.com/health-newsletter/Meniscus.htm↩︎
![AP Hip, AP Shoulder, and Axial Shoulder X-rays ^[http://medical-imaging2012.blogspot.com/2012/02/how-to-take-x-rays.html]](img/uncl/xray_HIP_AP.jpg)
![AP Hip, AP Shoulder, and Axial Shoulder X-rays ^[http://medical-imaging2012.blogspot.com/2012/02/how-to-take-x-rays.html]](img/uncl/xray_shoulder_normal1.jpg)
![AP Hip, AP Shoulder, and Axial Shoulder X-rays ^[http://medical-imaging2012.blogspot.com/2012/02/how-to-take-x-rays.html]](img/uncl/glenoid_axial.jpg)
![AP Hip, Oblique, and Lateral X-rays of the Foot ^[http://orthopedicgallery.com/portfolio/foot-x-ray/]](img/uncl/xray-Foot-AP-150x300.png)
![AP Hip, Oblique, and Lateral X-rays of the Foot ^[http://orthopedicgallery.com/portfolio/foot-x-ray/]](img/uncl/xray-Foot-oblique-165x300.png)
![AP Hip, Oblique, and Lateral X-rays of the Foot ^[http://orthopedicgallery.com/portfolio/foot-x-ray/]](img/uncl/xray-Foot-Lat-300x150.png)