3 Introduction
3.1 Course Introduction
Welcome to ME200: Orthopaedic Biomechanics
3.1.1 Introductions
- Please provide a brief introduction of yourself
- Name
- Degree in progress
- Ultimate degree goal
- Research topic and advisor (if grad student)
- Professional goals
- Optionally, an item or two of personal interest
- Note an online class makes it hard to develop relationships
- Professional networking is critical to job skill and opportunity growth
3.1.2 Objectives
The primary objective of this course is to present current methods for analysis of biomechanical systems that include bone, tendon, ligament, cartilage, and other soft tissue.
The relevant mechanics that govern biomechanical systems will be presented including elasticity, beam theory, anisotropic materials, viscoelasticity, and contact.
Additionally, prosthetics, orthotics, and other medical devices will be discussed.
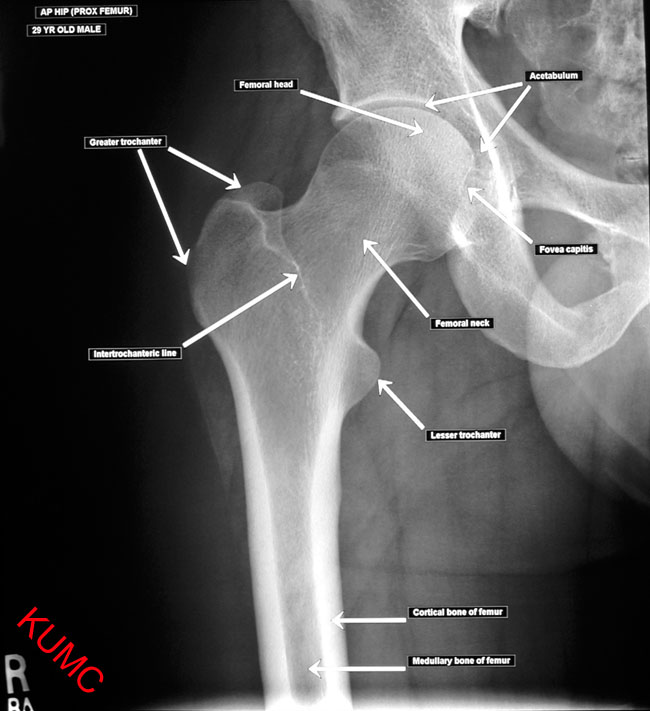
3.1.4 Almost-weekly anatomy quiz (Method TBD)
- Anatomy is an important part of orthopaedics
- We must be able to converse with medical personnel
- Thus, we will have an almost-weekly anatomy quiz
- The mechanism for doing this is still TBD (due to online-learning and Covid)
You will be assigned to watch a series of videos from AnatomyZone.com
http://anatomyzone.com/tutorials/basics/general-skeleton/
You will be assigned to watch those videos outside of the lecture period. Check elearning for more details.
3.2 Conceptual Overview of Orthopaedic Biomechanics
(Reading assignment: [@Bartel2006] Chapter 1.
3.2.1 The human body as a machine
- The human body is a machine!
- A combination of rigid and resistant bodies
- Bones and the soft tissue associated with them
- Links are joints which have low friction and transfer large forces
- Large, precise and imprecise motion
- Performs useful work
- A combination of rigid and resistant bodies
Contrasting humans with most machines
- Most joints have imprecisely defined motion
- There is flexibility in the soft tissues (ligaments, muscles)
- This flexibility leads to coupling between loads and motion:
- i.e. the motion can effect the loads in ways that do not typically occur in “conventional” machines
- Changes in force will produce changes in joint motion,
- Changes in relative position between bones (at joint) will change the forces in the joints
- “sloppy joint”
Joints, range of motion and, precision
- Hip joint
- is more rigidly defined by its bony ball and socket
- widely varying soft tissue restraint… but less reliance
- Shoulder joint
- is very imprecisely defined with its ball and socket
- widely varying soft tissue restraint…
- requires more soft-tissue control and precision placement

“Osteoporosis is the leading cause of age-related kyphosis, with sarcopenia, or age-related muscle loss, being a secondary cause,” Patel explains.2
- Skeletal loads vary from person to person and over time in a particular person
- Aging and disease change skeletal response
- We are not often concerned about precise loads, stresses, etc,
- rather we compute approximate loads within a level of uncertainty
- We seek to describe the fundamental behavior of the system
- Use engineering methods to understand the effect of damage and disease
- Predict, understand, and influence the methods and techniques used to restore function
- The skeleton has an amazing ability to repair damage and adapt to physical demands
Non-surgical treatment with a brace. Many humerus fractures can be treated without surgery. The humerus shaft fracture above was successfully treated in a “Sarmiento brace”, which wraps around the upper arm and holds the bone aligned while it heals.4

