ME5200 - Orthopaedic Biomechanics:
Lecture 3
Anatomy, functions of the musculoskeletal system, joints, soft tissue (continued)
Soft Tissue
Soft Tissue
- There are 4 types of soft tissue of interest to this course:
- Muscle
- Tendon
- Ligament
- Cartilage
- We will introduce each of these in this lecture, and each will get substantial treatment (lecture+)
Muscle

- Approximately 700 muscles in the human body
- Three broad classifications
- Skeletal
- Cardiac
- Smooth and visceral (internal to the body cavity)
- Also can be classified as
- Voluntary Striated (skeletal)
- Involuntary Striated (cardiac)
- Involuntary (smooth)
Muscle groups
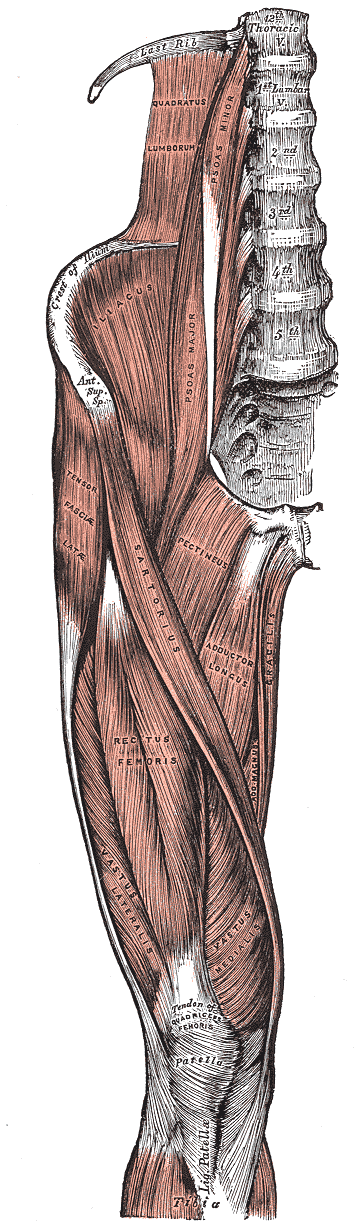
- In this course, we are principally concerned with skeletal muscles
- These muscles predominately act in groups that have a common insertion point on a bone
- The groups act in concert to provide motion and stability… we
will most often consider the group as a whole
- ie the quadriceps is made up of four muscles
- Muscles groups contract to activate, position, and stabilize the body
- They work in concert with each other, co-contraction of
agonist and antagonist muscles produces joint
control and stability
- Example, the hamstring and quadriceps simultaneously contract by variable amounts to stability the knee joint in flexion/extension

- Muscle contraction leads to forces, forces leads to strains in the
muscle
- Thus, the muscle is also a spring which stores energy
- This is important for energy management within the body
- Note the distinction between strain (injury) and strain (elasticity)
Tendons and ligaments

- Tendons connect muscle to bone
- Ligaments connect bone to bone
- Both can be modeled as simple cables, however, each has tissue bundles at multiple length scales (ie like fibers that join to form a strand, strands join to form a rope)
- When stretched, they deform and have spring like qualities as well
Articular cartilage
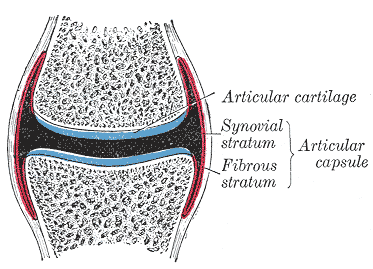
- Complex set of tissues consisting of fibrous matrix, water, large molecules, and other elements
- 2-4 mm thick… thickness changes with age
- Note: bursae - Tiny, slippery sacs of fluid which facilitate this gliding motion by providing a thin cushion and reducing friction between surfaces.2

- No nerves or blood supply in cartilage
- Difficult to detect damage
- Does not heal
- Level of detail in the engineering model depends on the desired outcome
Critical joints discussed in this course
The hip
- The hip is a synovial ball and socket joint.
- The head of the femur rotates relative to the acetabulum of the pelvis
- Contact can (sometimes) be modeled as a single force acting
through the center of the joint
- This approximation isn’t perfect
- Modeling the hip
- We might model the femoral diaphysis as a hollow circular beam
- The metaphysis can be modeled as an elastic or rigid link, or modeled using FEA if detailed outcome is desired
- Contact in the ball and socket leads to complex load distributions
- Muscle attachments to the greater and lesser trochanters
and bony ridges such as the linea aspera
- These allow for a greater moment arm for the muscles
The knee

- A bicondylar synovial joint which allows the femur and tibia to rotate, twist, and slide relative to each other
- Each motion is necessary… otherwise abnormal forces develop and cause rapid deterioration of the joint
- Important structures include:
- Medial collateral ligament (MCL)
- Lateral collateral ligament (LCL)
- Quadriceps tendon
- Patellar ligament
- Anterior Cruciate ligament (ACL)
- Posterior Cruciate Ligament (PCL)
- Menisci (two crescent-shaped pads that help distribute the loads from the femoral condyles to the tibial plateaus)
- ACL and PCL are within the knee joint capsule and pass through the notch between the condyles, the others are outside the capsule
Spine

“Cartilaginous” type joint
Connective tissue is a fibrocartilage structure called the Intervertebral disc
Healthy disk acts like a tire… needs to have sufficient fluid inside.
- Aging causes the gel-like fluid to solidify with negative consequences
- Largest avascular tissue in the body
Anterior portion of the intervertebral joint
- Pedicles and laminae form an arch – the vertebral foramen (hole) for the spinal cord


- Adjacent vertebrae are connected through articulating joints (called facets) that constrain the motion between the vertebrae and limit twisting and extension of the spinal column
- The structure supports the upper body and protects the spinal cord.
Vertebral attachments
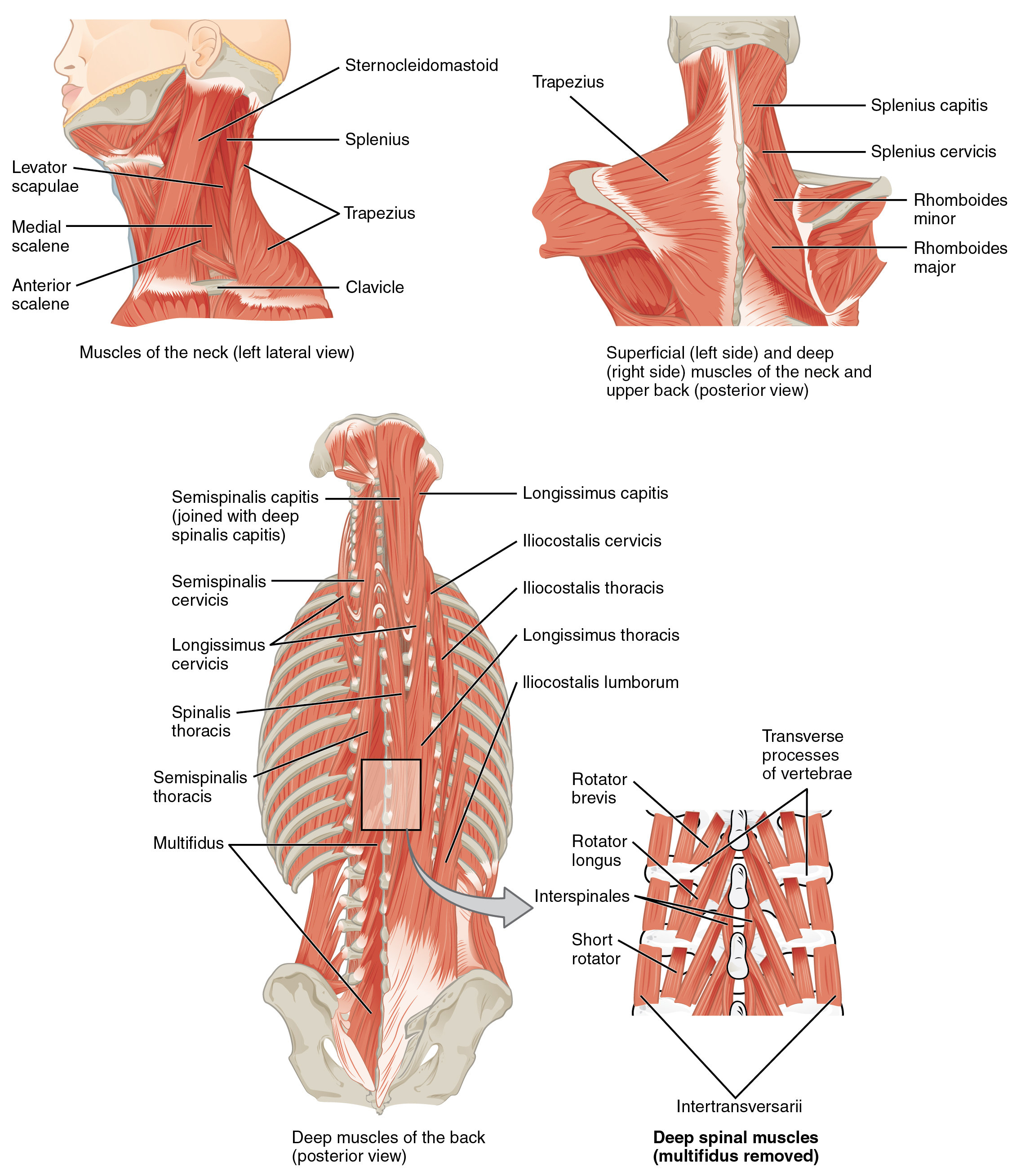
- Back muscles attach \(\approx 5\)cm posterior to the center of the vertebral body
- Center of sagittal bending is approximately within the disk
Latissimus dorsi

Fracture
WARNING: Traumatic video coming
Fracture
Fractures may occur due to:
- Abnormal loading
- Single traumatic overload
- Cyclic loading which does not overload but prevents healing
- ie stress fracture
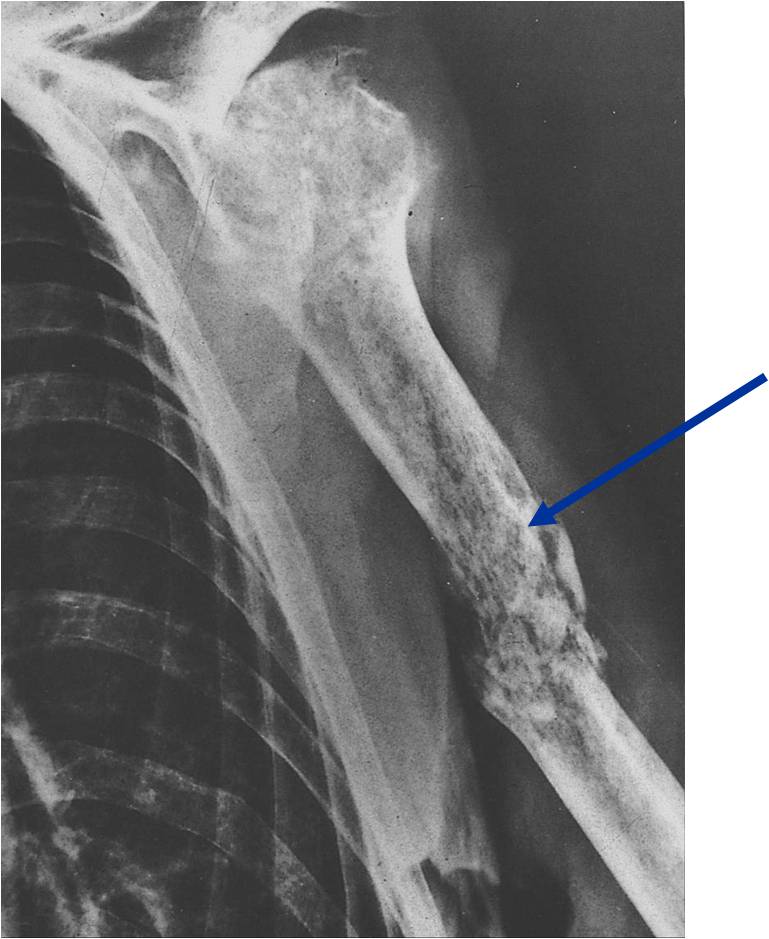
- Decreased strength due to underlying pathology
- Tumors
- Disease (osteoporosis)
- Lack of use
- Adaption to load demand – prolonged bed red, paralysis, reduced gravity environment, stress shielding by an implant
- Possible project… investigate mathematical models of bone adaptation
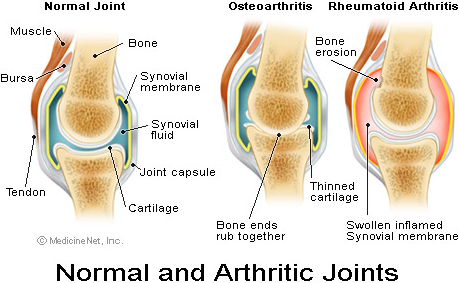
Arthritis
Arthritis
- Deterioration of the joints over time
- Osteoarthritis occurs when some combination of mechanical wear and biochemical degradation erodes the articular cartilage
- It is a localized effect most common in knees and hips
- Damage to articular cartilage may be caused by normal wear, disease, or trauma
- Damage may be direct or due to changes in the subchondral bone
- May also be caused by altered joint mechanics
- ie change in gait due to ankle fusion leads to arthritis in the knee
- Damage may be caused by systemic disease
- Rheumatoid arthritis
Soft tissue damage
- Traumatic loads may cause ruptures of ligaments, tendons, and the menisci
- Damage may occur in the ligament/tendon itself or in the attachment
point to the bone or muscle
- May be entirely within the bone
- The nature of the injury can depend on the rate of loading
- Tendons/ligaments exhibit viscoelastic behavior
Repair
- Musculoskeletal system has an extraordinary ability to repair itself (if the damage is not too severe)
- Bone is continually “damaged” and continually repairs itself
- Damage may be related to the adaption process and necessary to maintain bone density
- Self repair varies with site, tissue, and extent of the injury
- Bone is good at self repair
- Muscle, tendon, and ligament are not as good at self repair
- Severe damage may necessitate medical or surgical intervention
Visualizing orthopaedic structures
X-Ray of a Hand

High energy electromagnetic radiation allows the internal structures of the body, such as bones, to be seen in X-rays like these. (credit: Trace Meek/flickr)
(slide credit: @OpenStaxAnatomy2020 Ch. 1)
Computed Tomography Scan

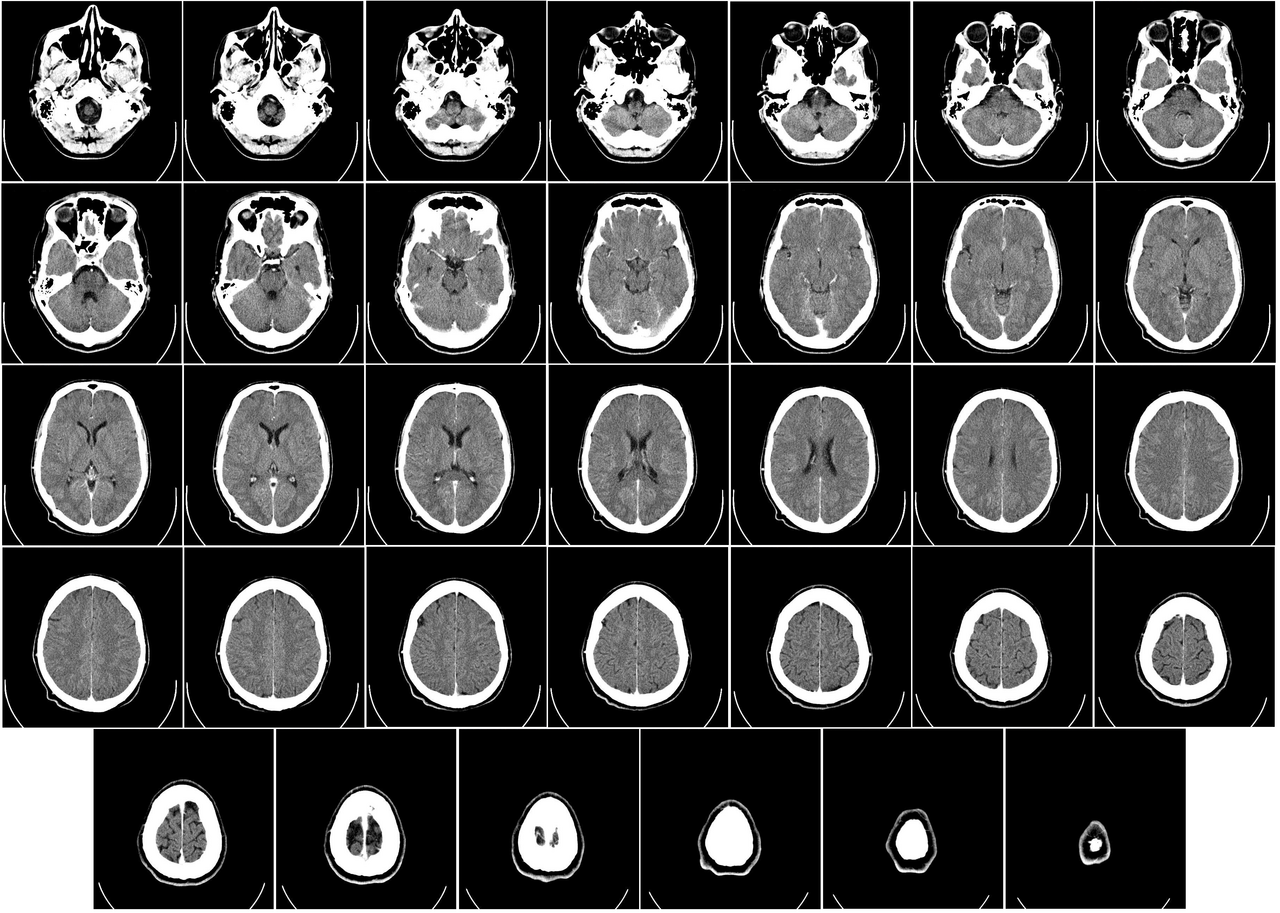
- The results of a CT scan of the head are shown as successive transverse sections.
- Uses ionizing radiation (x-ray radiation)
- Higher contrast visualization of bony structures
Magnetic Resonance Imaging


- An MRI machine generates a magnetic field around a patient.
- Higher contrast visualization of soft tissues
Ultrasound

Ultrasonography is a totally safe noninvasive imaging technique. In contrast to computed tomography (CT) and X-rays, it does not emit ionizing radiation. Unlike magnetic resonance imaging (MRI), it is safe for all patients, including those with cardiac pacemakers and metal implants, without any contraindications.
@Blankstein2011
Ultrasound in orthpaedics
- Can be high resolution
- Can offer real time assessment (i.e., patient can move, image is dynamic)
- Sometimes referred to as the “orthopedic surgeon’s stethoscope”
- Detection of tendon tears, tiny calcifications, and foreign bodies
Positron emission tomography
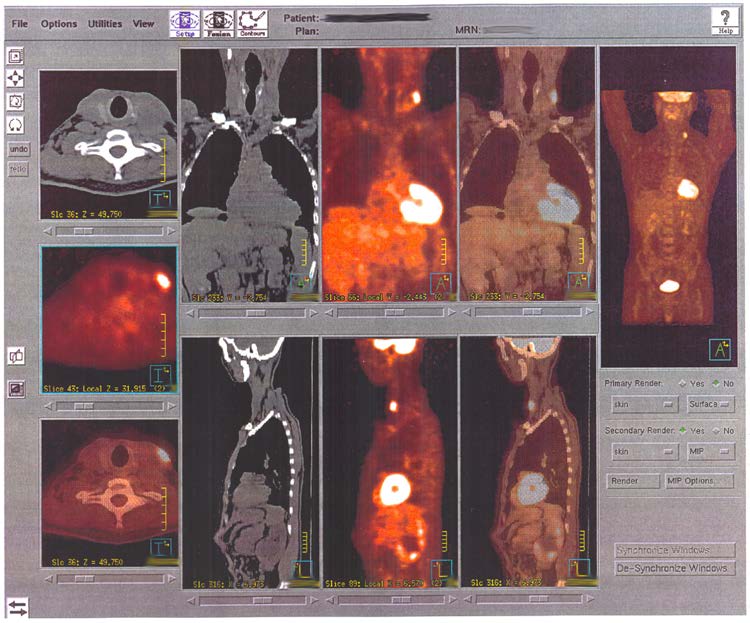
PET highlights areas in the body where there is relatively high glucose use, which is characteristic of cancerous tissue. This PET scan shows sites of the spread of a large primary tumor to other sites.
(slide credit: @OpenStaxAnatomy2020 Ch. 2)
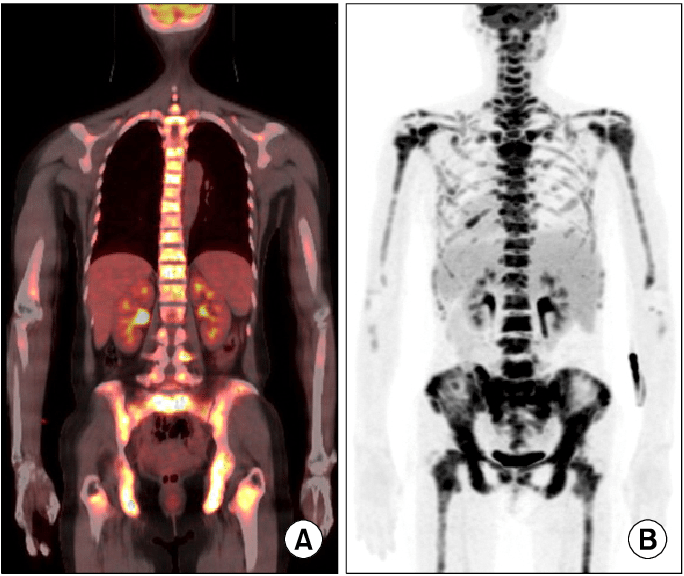
- Can be used to track bone forming activity
Summary
Objective
To understand the musculoskeletal system well enough to provide engineering support for the treatment of musculoskeletal disorders and for the enhancement of individual and societal quality of life
- Thus, we must:
- understand the basic mechanics or normal, damaged, and repaired tissue and the body structures composed of them
- utilize modern design and analysis tools to improve treatment of disorders